Photo Credit: Courtesy of Ground Picture/ShutterstockDo you find yourself struggling with a recurring pattern of unwanted thoughts and fears, which lead you to engage in repetitive behaviors? For example, washing your hands every time you touch a door handle, brushing your teeth after every meal, or avoiding stepping on sidewalk cracks? These are common manifestations of obsessive-compulsive disorder (OCD), a condition that can cause distress and anxiety in your life.
Photo Credit: Courtesy of Ground Picture/ShutterstockDo you find yourself struggling with a recurring pattern of unwanted thoughts and fears, which lead you to engage in repetitive behaviors? For example, washing your hands every time you touch a door handle, brushing your teeth after every meal, or avoiding stepping on sidewalk cracks? These are common manifestations of obsessive-compulsive disorder (OCD), a condition that can cause distress and anxiety in your life.
According to the Mayo Clinic, individuals with OCD may attempt to ignore or suppress their obsessions, but doing so often results in increased distress and anxiety. Despite your efforts to avoid these urges, they tend to resurface, making it challenging to break free from the cycle of ritualistic behaviors. At Gut Feelings Psychiatry, we understand the impact of OCD on your life, and we offer a range of therapies tailored to treat this condition. Our center is dedicated to helping you find relief from OCD symptoms. We provide various evidence-based therapies to address the root causes of your obsessions and compulsions.
In some cases, individuals with OCD may not respond adequately to traditional therapies, leading to the consideration of alternative options. If you happen to be treatment-resistant, we offer transcranial magnetic stimulation (TMS) as an advanced therapeutic approach. Let’s dive into what TMS is and how it can potentially benefit you.
What is Transcranial Magnetic Stimulation (TMS), and how does it work to treat treatment-resistant depression and OCD?
TMS (Transcranial Magnetic Stimulation) uses magnetic fields to stimulate nerve cells in the brain, specifically in areas associated with mood regulation and emotional processing. It works by delivering magnetic pulses to the prefrontal cortex, a region linked to mood regulation. This area can be stimulated with TMS to improve symptoms and normalize neuronal activity. It is FDA-approved to treat depression and obsessive-compulsive disorder (OCD).
What are the typical treatment protocols for TMS in these conditions?
TMS usually involves daily sessions over several weeks for treatment-resistant depression and OCD. In most cases, TMS is done five days a week for four to six weeks. Sessions last about 20 to 30 minutes.
What are the potential benefits of TMS compared to other treatment options for treatment-resistant depression and OCD?
Treatment-resistant depression and OCD patients may benefit from TMS due to its noninvasive nature and reduced side effects compared to medications and electroconvulsive therapy (ECT). TMS also offers a targeted approach, specifically addressing the affected areas of the brain, which can lead to significant improvement in quality of life.
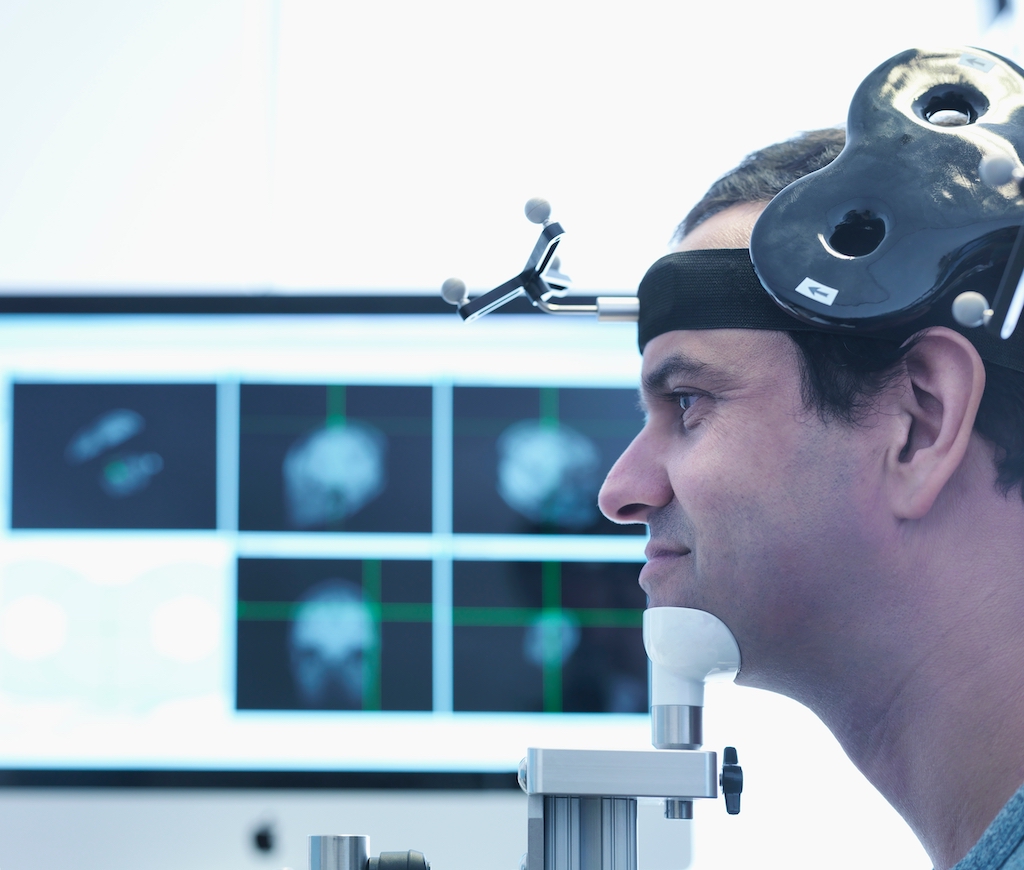 Photo Credit: Courtesy of Image Source Trading Ltd/Shutterstock
Photo Credit: Courtesy of Image Source Trading Ltd/Shutterstock
How do you determine if I am a suitable candidate for TMS? What are the criteria for eligibility?
Whether a patient is a suitable candidate for TMS is based on several factors. To qualify for insurance coverage, typically patients must have failed multiple medications. And we don’t perform TMS on people with certain psychiatric or neurologic conditions. Metal implants in the head, for example, are contraindications for TMS.
Are there any medical conditions or medications that could interfere with TMS treatment or make it less effective?
Yes, certain medical conditions, such as epilepsy or seizure disorders, and specific medications may interfere with TMS treatment or make it less effective. It is important to undergo a comprehensive evaluation and inform your healthcare provider about your medical history and medications before starting TMS therapy.
Can TMS be used in combination with other therapies or medications for depression and OCD?
Yes, TMS can be used in combination with other modalities. Your psychiatrist will work with you to develop a personalized treatment plan that may include a combination of TMS, psychotherapy, and medications to work toward your therapeutic goals.
How soon can I expect to see improvements in my symptoms after starting TMS treatment?
The time it takes to see a response can vary from person to person. Some individuals experience positive changes early in the treatment course, while others may take a few weeks to notice significant improvements. Patience and consistency with the visits are essential.
What is the success rate of TMS in treating treatment-resistant depression and OCD, and how is “success” defined in this context?
The success rate of TMS in treating treatment-resistant depression and OCD is quite promising. Success is typically defined as a significant reduction in symptoms and an improvement in the patient’s overall quality of life. Studies have shown that TMS can have a positive impact on a substantial number of patients who have not responded well to other treatments, offering new hope for those struggling with these challenging conditions. Clinical outcomes from a large TMS registry demonstrate that 83% of patients experience improvement in symptoms and 62% achieve remission.
It’s important to consult with a qualified psychiatrist or healthcare professional to determine the most suitable treatment approach for your specific needs and to undergo a comprehensive evaluation to assess your eligibility for TMS therapy.
For more information, visit Dr. Brian A. Levine's social media: