Widely considered one of the top fertility experts in the field, Dr. Mark Surrey has been in practice for over 25 years. He is a board-certified reproductive and endoscopic surgeon and serves as a clinical professor in the Department of OBGYN at UCLA’s David Geffen School of Medicine. He was elected President of the American Laparoscopy Society & Pacific Coast Reproductive Society and is a Clinical Director of Fellowship Training for UCLA & Cedars Sinai Reproductive Endocrinology. Also a founding member of The Society of Reproductive Surgeons. Dr. Surrey is a yearly recipient of the leading research contributions for ASRM. Furthermore, he is the associate director at the Southern California Reproductive Center, a clinic he co-founded. Haute MD sits down with Dr. Mark Surrey to discuss a preimplantation genetic diagnosis procedure to evaluate any potential genetic defects within the embryo.
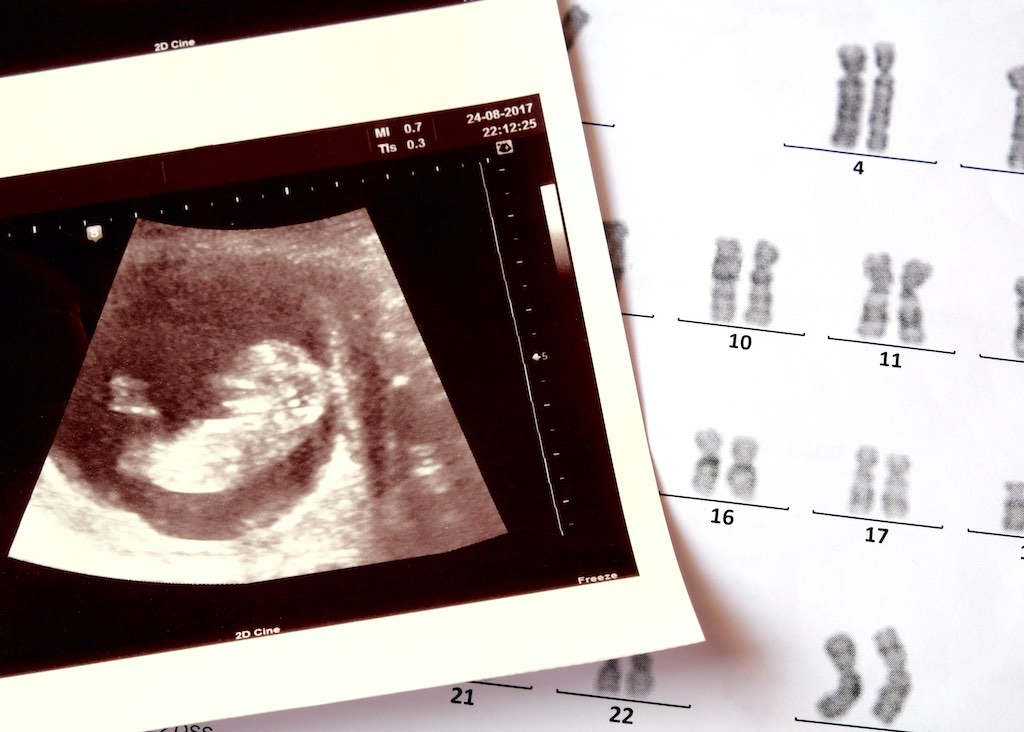 Photo Credit: ShutterstockHaute MD: What is a preimplantation genetic diagnosis?
Photo Credit: ShutterstockHaute MD: What is a preimplantation genetic diagnosis?
Preimplantation genetic diagnosis or PGD is a procedure used prior to embryo implantation to help identify genetic defects within the embryo. This serves to prevent certain genetic diseases or disorders from being passed on to the child and the diagnosis is a complete chromosome analysis that includes gender.
Haute MD: What type of indicators are you looking for?
The utility of this information will improve the chances of a healthy baby and decrease the miscarriage rate. A variety of genetic diseases can be ruled out, such as monogenic (single-gene) disease, chromosomal abnormalities, mitochondrial disorders, or complex disease. The accuracy of this is efficient & accurate.
Haute MD: How does the treatment process work?
The PGD process requires several steps, each performed by a different expert or laboratory. You begin with the in-vitro fertilization (IVF) by which an embryo is produced. Fertilized embryos are then cultured for 3-5 days. Biopsies of the embryo are done on day 5 and the results usually are available in about 24 hours. Often the embryos are frozen through vitrification, a rapid freeze method to make sure no harm will come to them while the patient and doctor await the results. The healthy, normal embryo will then be thawed in the final stage and implemented in the mother via embryo transfer.
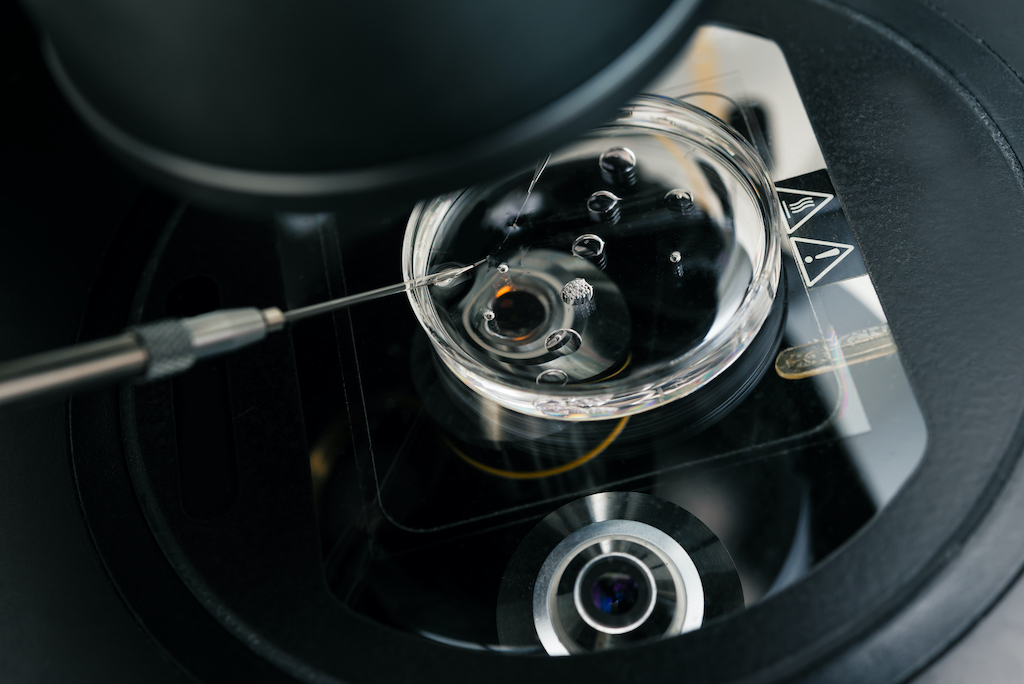 Photo Credit: ShutterstockHaute MD: Who are the prime candidates for this diagnostic test?
Photo Credit: ShutterstockHaute MD: Who are the prime candidates for this diagnostic test?
Today it is information that is essential prior to an embryo transfer so I and my fellow colleagues at SCRC recommend every patient to get tested. It is highly advisable for couples or individuals with known genetic disorders are advised to test prior to embryo implementation. It is also recommended for women with recurrent miscarriages or multiple failed fertility treatments to test, as well as women of advanced maternal age.
Haute MD: What's next after results are determined?
Once the results are in, the test will reveal whether the embryo is normal or euploid, abnormal or mosaic, meaning some of the embryo's cells showed normal, other abnormal results. If an embryo’s cells show abnormality (or a mosaic structure), the patient and doctor will need to discuss the chances of a successful pregnancy and what birth defects a parent will have to expect. It is then up to the parent(s) to make a choice about implementing the embryo.
For more information, visit Dr. Mark Surrey's social media: